Adult Civil Mental Health
This page includes tools, resources, and information for judicial officers, court staff and justice system partners related to adult civil mental health in the courts. Visit the CARE Act page on the self-help guide for more information.
CARE Act

The Community Assistance, Recovery, and Empowerment (CARE) Act authorizes specified adult persons to petition a civil court to create a voluntary CARE agreement or a court-ordered CARE plan that can include treatment, housing support, and other services for persons with schizophrenia or other psychotic disorders. The CARE Act creates a new pathway intended to deliver mental health treatment and support services upstream to the most severely impaired Californians who often experience homelessness or incarceration without treatment. This pathway is accessed when a person, called the “petitioner”, requests court-ordered treatment, services, support, and housing resources under the CARE Act prioritized for another person, called the “respondent”. The petitioner must fall under a specific group of people, such as specific family members, housemates, first responders, and behavioral health workers. The respondent must have a diagnosis on the schizophrenia spectrum or other psychotic disorders.
As of December 2024, all courts and counties have implemented the CARE Act.
The CARE Act Implementation in the California Courts webpage displays statewide CARE Act data elements reported by the courts.
Who Can Be a Respondent?
To be eligible for CARE Act proceedings, the individual must meet all the following criteria:
- Be 18 years old or older
-
Have a diagnosis of schizophrenia spectrum disorder or other psychotic disorder, or bipolar I disorder with psychotic features, except psychosis related to current intoxication
- Be currently experiencing a mental illness that is severe in degree and persistent in duration, which may cause behavioral functioning which interferes substantially with the primary activities of daily living, and which may result in an inability to maintain stable adjustment and independent functioning without treatment, support, and rehabilitation for a long or indefinite period of time
- Not currently clinically stabilized in an on-going voluntary treatment program
- Meet one of the following:
- The person is unlikely to survive safely in the community without supervision and the person’s condition is substantially deteriorating.
- The person is in need of services and supports in order to prevent a relapse or deterioration that would likely result in grave disability or serious harm to the person or others, as defined in Section 5150.
- CARE would be the least restrictive alternative to ensure the person’s recovery and stability
- Be likely to benefit from participation in CARE
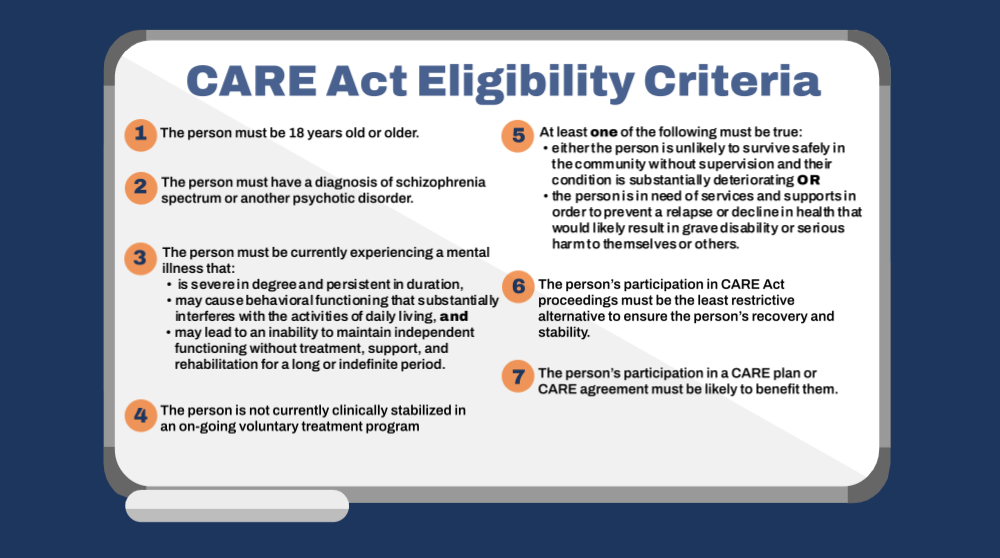
This five-minute video walks through the seven eligibility criteria that must be met in order for someone to be eligible for services under the CARE Act.
Who Cannot Be a Respondent?
Certain conditions and disorders are excluded, including:
- Serious mental illnesses outside of psychotic disorder class, including bipolar II disorder, major depression, and post-trauma stress disorder
- Psychotic disorders due to medical conditions, such as traumatic brain injury, autism, dementia, or other physical health or neurological conditions
- Substance use disorder that does not otherwise meet the definition of a psychotic disorder
Who Can Be a Petitioner?
To be a petitioner, you must be 18 years of age or older. You can be related to the respondent or be the director of an agency who has had frequent contact with the respondent due to their mental health disorder. You must fall within one of the following categories to be able to request CARE Act proceedings for a respondent:
- A person who lives with the respondent
- A spouse or registered domestic partner, parent, sibling, child, or grandparent of the respondent
- A person who stands in the place of a parent to the respondent
- The director of certain county agencies, specifically adult protective services, a county behavioral health agency, or the public guardian or public conservator, or that person’s designee
- The director of a hospital, or their designee, in which the respondent is hospitalized
- A licensed behavioral health professional or director of a public or charitable agency, who is currently or has been recently treating, or supervising the treatment of, or providing behavioral health services for the respondent within the last 30 days
- A first responder who has had repeated interactions with the respondent
- A judge of a tribal court located in California, before which the respondent has appeared within the previous 30 days, or the judge’s designee
- The director of a California Indian health services program or a California tribal behavioral health department, who has, within the previous 30 days, provided or who is currently providing behavioral health services to the respondent, or the director’s designee
- The respondent themself
When Did the CARE Act Start?
California rolled out implementation of the CARE Act in phases:
- 7 counties (Glenn, Orange, Riverside, San Diego, San Francisco, Stanislaus, Tuolumne) implemented on October 1, 2023.
- Los Angeles implemented on December 1, 2023.
- San Mateo implemented on July 1, 2024.
- Kern implemented on October 1, 2024.
- Mariposa implemented on November 1, 2024.
- Napa implemented on November 25, 2024.
- The remaining 46 counties implemented by December 1, 2024.
CARE Act Toolkit:
The CARE Act Toolkit includes informational documents about implementation and eligibility. Additional documents will be posted here as they are developed.
- CARE Act Fact Sheet (February 2026) - Older versions also available in: Chinese, Farsi, Korean, Spanish, and Vietnamese
- Glossary of CARE Act Terminology - Also available in: Chinese, Farsi, Khmer, Korean, Spanish, Tagalog, and Vietnamese
- CARE Act Eligibility Criteria - Also available in: Chinese, Farsi, Korean, Spanish, and Vietnamese
- 10 Things to Know About the CARE Act
CARE Act Petitions:
The following resources include information about CARE Act proceedings and assist petitioners and respondents with the filing of petitions. For direct support, find your local self-help center to get answers to questions and receive help completing and filing a petition. CARE Act forms are available in Chinese, Korean, Spanish, and Vietnamese and can be accessed by clicking the links below.
- CARE-050-INFO (Information for Petitioners-About the CARE Act)
- CARE-060-INFO (Information for Respondents-About the CARE Act)
- CARE-100 (Petition to Begin CARE Act Proceedings)
- How to File the CARE-100
- CARE-101 (Mental Health Declaration-CARE Act Proceedings)
- CARE-113 (Notice of Respondent’s Rights-CARE Act Proceeding)
CARE Act Webinars:
The following webinars are hosted by CFCC and include curated interdisciplinary content related to CARE Act implementation.
CARE Act 101 Webinar: Overview of the Court’s Role in Implementation
The CARE Act 101 webinar provides an overview of the court’s role in implementation and highlights key topics and spotlights areas of greater interest for local courts and justice partners including eligibility criteria, referrals, and the court process. The presentation is approximately 30 minutes.
CARE Act Judicial Process Overview Training for Counsel
This session provides an in-depth overview of the CARE Act judicial process and highlights the eleven new rules and thirteen new forms created by the Judicial Council for counsel, including public defenders, qualified legal services projects, and county counsel.

Effective Communication for Court Users with Psychiatric Disabilities
Disability Rights Education and Defense Fund provides a one-hour training on effective communication and reasonable modifications for court users with psychiatric disabilities, including people with schizophrenia and other thought disorders.

Confidentiality and the CARE Act: A Primer
This session provides and overview of the fundamentals of confidentiality law with regard to adult civil mental health proceedings, with a focus on the CARE Act. The session covers HIPAA the Confidentiality of Medical Information Act (CMIA), the confidentiality provisions of the Lanterman-Petris-Short (LPS) Act and the Comprehensive Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act (CAAAPTR), as well as those included within the CARE Act itself.
Are There Other Options if CARE Act Proceedings Don’t Make Sense for Me or My Loved One?
Yes. You can contact your county behavioral health agency to discuss additional options. These may include voluntary services, such as full-service partnerships, assertive community treatment, or supportive housing, or court-ordered services, such as Assisted Outpatient Treatment (AOT) or services under the Lanterman-Petris-Short Act (LPS). Scroll down to learn more about AOT and LPS.
Questions about CARE Act implementation? Please email care.act@jud.ca.gov.
Additional information is available from the California Health and Human Services Agency CARE Act webpage as well as the California Department of Health Care Services website.
Laura’s Law / AOT
Assisted Outpatient Treatment, known as Laura’s Law, allows for court-ordered assisted outpatient treatment for defendants with serious mental illness who are unable to survive safely in the community without supervision. Laura’s Law permits counties to utilize courts, probation, and mental health systems to address the needs of individuals who meet certain criteria, including those with a history of repeated hospitalization or incarceration, or a history of violent behavior to self or others. Under Assembly Bill 1976 (Stat. 2020, ch. 140), counties were required to formally opt-in or opt-out of Laura’s Law by July 1, 2021, encouraging new counties to begin implementing court-ordered assisted outpatient treatment.

Due Process in Assisted Outpatient Treatment (“Laura’s Law”): Common Issues and Questions(1:03:37)
Laura’s Law provides court-ordered Assisted Outpatient Treatment for people with a history of violence or repeated hospitalizations and who are unable to participate in mental health treatment programs without supervision. This webinar discusses common due process issues, problem-solving, and county-specific experiences. Topics include adequacy of notice, confidentiality, waiver of rights, and enforcement mechanisms.
Lanterman-Petris-Short (LPS) Act
California’s civil mental health law is the Lanterman-Petris-Short Act, or LPS, named after the three legislators who originally drafted the legislation. Designed to, among other things, “end the inappropriate, indefinite, and involuntary commitment of persons with mental health disorders, developmental disabilities, and chronic alcoholism,” “provide prompt evaluation and treatment,” and “safeguard individual rights through judicial review,” the law sets out procedures for involuntary treatment and protects patients’ rights.
For more information on the LPS Act:
- Assembly Hearing Background Materials - The Lanterman-Petris-Short Act: How Can it be Improved?
- Understanding the LPS Act - Disability Rights California